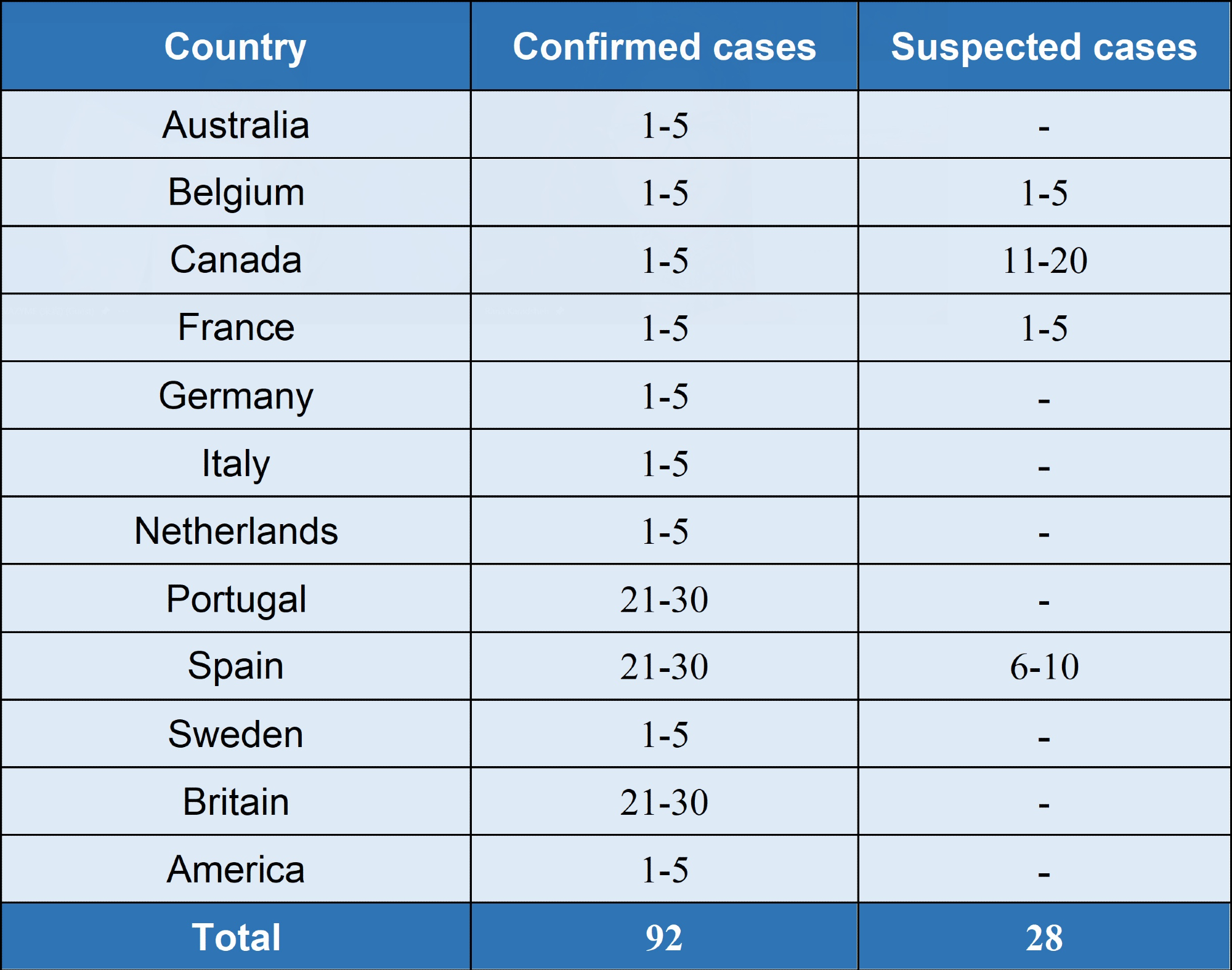
As of the United Nations bulletin on May 22nd, 2022, there have been 92 confirmed cases and 28 suspected cases in 12 non-monkeypox virus endemic countries around the world since May 13th (Table 1 for details) as reported by the World Health Organization (WHO). So far, there have been no related deaths.
Table1. Monkeypox cases in non-endemic countries reported to WHO from 13:00 on May 13 to 21, 2022. Source: Vazyme Biotech Co. Ltd.
From December 15th, 2021, to May 1st, 2022 (as shown in Table 2), there have been four African countries with a monkeypox epidemic which have reported 1315 confirmed cases to WHO. There is no travel history in endemic countries among the currently reported confirmed and suspected patients in non-endemic countries.
To date, existing cases have largely been found among men who have sex with men. People who have close physical contact with symptomatic cases are likely to catch the virus, and this mode of transmission is likely to be partly responsible for the spread.
Table 2. Monkeypox cases in endemic countries from December 15, 2021, to May 1, 2022. Source: Vazyme Biotech Co. Ltd.
| COUNTRY | TIME PERIOD | ACCUMULATED CASES | ACCUMULATED DEATH |
|---|---|---|---|
| Cameroon | December 15,2021 to February 22,2022 | 25 | <5 |
| Central African | March 4 to April 10, 2022 | 6 | <5 |
| Congo | January 1 to May 1, 2022 | 1238 | 57 |
| Nigeria | January 1, 2022, to April 30, 2022 | 46 | 0 |
Introduction to monkeypox virus
Monkeypox virus: what is it?
Monkeypox virus belongs to the Orthopoxvirus genus of the Poxviridae family and is an enveloped double-stranded DNA virus. The monkeypox virus has two distinct genetic clades: the west African clade and the central African (Congo Basin) clade. Cameroon is, to date, the only country where both virus clades have been found concurrently.
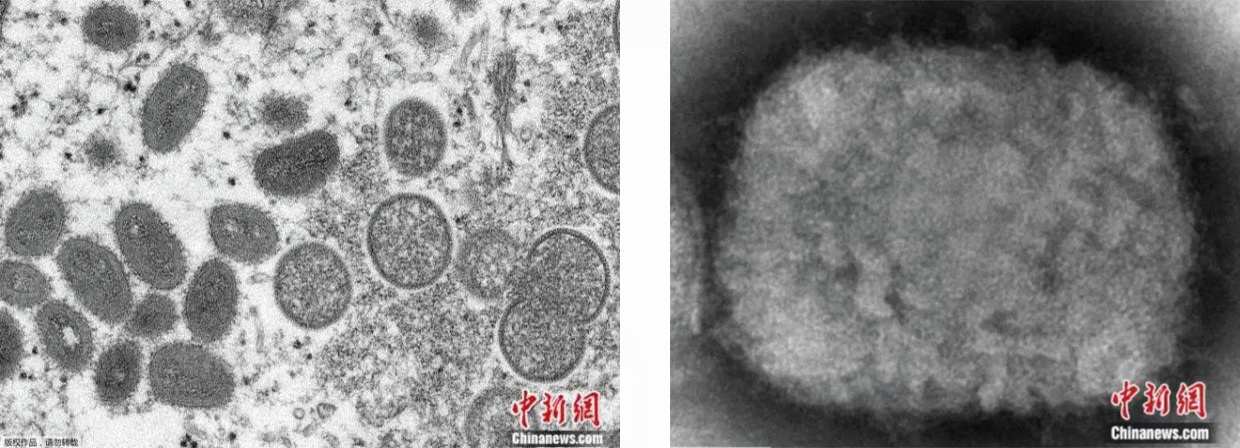
Figure 1. The structure map of monkeypox virus. Image Credit: Chinanews.com
Monkeypox virus: Symptoms
Monkeypox has emerged as the most important orthopoxvirus for public health, with the eradication of smallpox in 1980 and subsequent cessation of smallpox vaccination.
As a zoonotic orthopoxvirus, monkeypox has an incubation period of 6 to 13 days. It is characterized in the early stages by intense headache, lymphadenopathy (swelling of the lymph nodes), fever, muscle aches, and intense asthenia.
A few days after fever, typical systemic purulent herpes usually begins, which can lead to secondary infection. Within the general population, the fatality ratio of monkeypox has ranged from 0 to 11 % and has been found to be higher among young children.

Image Credit: Picture uploaded by NetEase Hao netizen
Transmission and diagnosis
Transmission
Damaged skin, respiratory tract or mucous membrane (eyes, nose or mouth) can all be modes of monkeypox virus transmission. The three main modes of transmission are:
- Animal-to-human transmission (this involves direct contact with the bodily fluids, blood, or cutaneous lesions of an infected animal, including bites or scratches).
- Human-to-human transmission (this involved close body contact with patients who are infected);
- Contaminated-object-to-human transmission (this involves contact with the patient’s bodily fluid, respiratory droplets, focus, or contaminated materials such as bedding)
The typical incubation period of the monkeypox virus is 6 to 13 days but can be as many as 21 days. It was reported both in local media and national outlets like The Guardian and local media reports on the 22nd that the British health and safety agency has proposed that anyone discovering that they have had close contact with or are living together with confirmed cases of monkeypox should self-isolate for 21 days.
It is vital that monkeypox is diagnosed in good time to inhibit the spread and minimize the impact.
Diagnosis
The first step of diagnosis is the clinical identification of monkeypox. This confirmation of monkeypox requires a range of different laboratory tests, including virus isolation from cell culture, polymerase chain reaction (PCR) analysis, antigen detection test and an enzyme-linked immunosorbent assay (ELISA).
It is important to note that monkeypox-specific confirmation is not provided by antigen and antibody detection methods due to the serological cross-reactivity of orthopoxviruses. Therefore, in investigations where resources are limited, antigen and serology detection methods are not recommended for diagnosis or case.
The existence of the virus can only be confirmed by PCR and virus isolation from cell culture. Of these, PCR is the preferred laboratory test as a result of its sensitivity and accuracy. Vesicles, blood specimens, pustular fluid, and scab specimens all provide samples of monkeypox, but the optimal diagnostic is from skin lesions – the fluid or roof from vesicles and pustules, as well as dry crusts.
Vazyme: Providing the solution
Many IVD companies have developed monkeypox virus nucleic acid detection kits since the outbreak of the monkeypox virus. Vazyme, as a supplier of professional solutions and raw materials within the fields of biomedicine, life science, and in vitro diagnosis, is able to provide clients with a full set of solutions.
These solutions include positive control, amplification reagents, and primer probe design, all of which are required for product development when attempting to generate monkeypox diagnosis to help clients rapidly complete their product development.
Nucleic acid amplification
Table 4. Source: Vazyme Biotech Co. Ltd.
| PRODUCT CLASSIFICATION | ITEM NUMBER | NAME | PRODUCT INTRODUCTION | |
|---|---|---|---|---|
| Enzyme mix | qPCR mix | QN213 | Taq Pro U+ Multiple Probe qPCR Mix | qPCR premix with wide compatibility, support rapid amplification, high sensitivity and high specificity |
| QV114 | Animal Detection U+ Probe qPCR Super PreMix | Highly sensitive qPCR premix, support full premixing of primer probes, compatible with rapid procedures |
Image Credit: Vazyme Biotech Co. Ltd.
After monkeypox cases exploded last month in countries such as Portugal, Spain and the United Kingdom — where outbreaks don’t usually occur — a rapid, global response followed, including the distribution of vaccines in some countries. Some researchers in parts of Central and West Africa, where monkeypox outbreaks have been occurring for years, are disheartened that such resources have not been made available in their countries. They have long been warning of the potential for the monkeypox virus, which has been behaving in new ways, to spread more widely. “Isolated solutions that fix the problem for developed countries alone and leave out developing countries will lead us through the same cycle again,” says Dimie Ogoina, an infectious-disease physician in Nigeria. “It’s just a matter of time.”